Fentanyl Withdrawal Symptoms, Timeline, & Detox Treatment Options
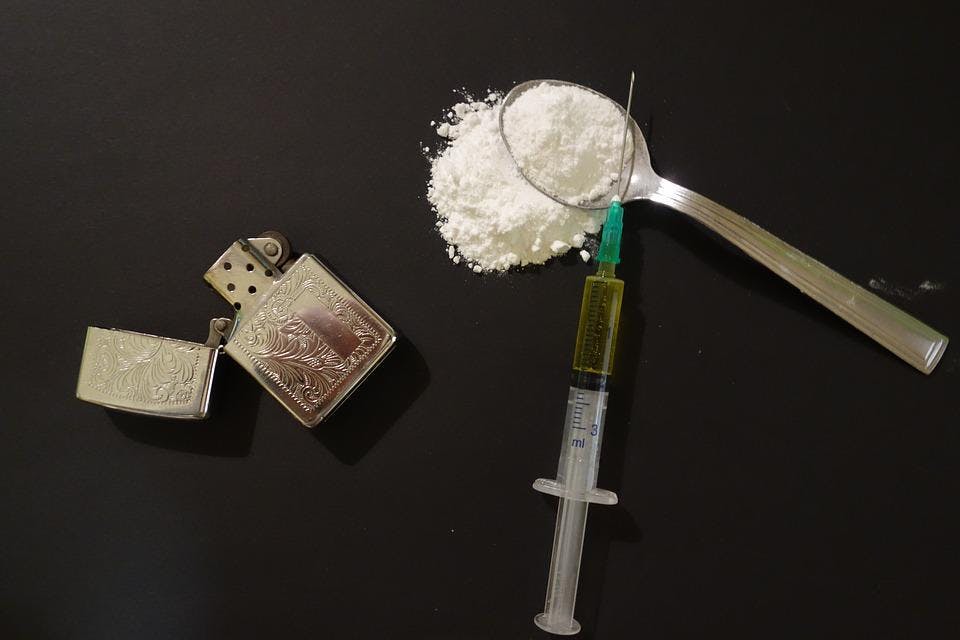
Fentanyl is a powerful synthetic opioid 80-100 times stronger than morphine. Initially developed for pain management, specifically for cancer patients, this drug has created a wave of drug abuse — fueling the current opioid crisis.
There have been three distinct waves concerning opioid overdose deaths. The first began in the 1990s, involving prescription opioids. The second wave began in 2010, with a rapid increase in overdose deaths involving heroin. Most recently, the third wave involves synthetic opioids, particularly fentanyl.
Data from the CDC shows that over 70% of overdose deaths in 2019 involved an opioid. Overdoses involving opioids killed nearly 50,000 people that year, and almost 73% of those deaths involved synthetic opioids.
Opioids create significant withdrawal symptoms, and while they are uncomfortable, continuing to use them is incredibly dangerous. There are programs available to help you overcome the initial withdrawal symptoms to focus on the next steps. The road to recovery is often a marathon, not a sprint. However, when you have an expert team to assist you, they will provide you with the support and resources you need to succeed.
If you or your loved one are struggling with fentanyl or other opioids, you do not need to fear the withdrawal process. Help is available. Here is everything you need to know about the fentanyl withdrawal process. Plus, how to take the first step toward a healthier, more fulfilling future.

What Are the Symptoms of Fentanyl Withdrawal?
The effects of fentanyl are similar to those of heroin, and so are fentanyl withdrawal symptoms. These symptoms are a significant barrier to treatment. Most users attempt to complete the fentanyl withdrawal process at home, and once symptoms peak, they use it to avoid feeling substantial discomfort.
Withdrawing from any opioid, including fentanyl, is often very uncomfortable and difficult. The symptoms that develop often cause users to relapse and are often compared to a bad flu. Although there are circumstances where fentanyl withdrawal can be dangerous, opioid withdrawal is not typically life-threatening. In most cases, users can safely withdraw from fentanyl.
However, research shows that under certain circumstances, opioid withdrawal is fatal. Some industry experts believe that complications of opioid withdrawal are often underestimated and not adequately monitored. In most cases, fatalities occur in prison settings, where vomiting and diarrhea result in severe dehydration and death.
Fatalities are the exception, not the rule — but that does not mean you should attempt to withdraw on your own. Most users will experience symptoms that make it hard not to take the next dose. When beginning the fentanyl withdrawal period, to ensure you have the greatest chances of success, it’s recommended that you complete the process in a controlled, supervised environment.
The most common symptoms you will experience during fentanyl withdrawal include:
- Nausea and vomiting
- Anxiety
- Insomnia
- Sweating
- Muscle cramps
- Hot and cold flashes
- Diarrhea
- Tremors
- Confusion
The severity of the above symptoms will depend on the dose and withdrawal speed. For example, if you have been taking high doses for an extended period and then quit cold turkey, you can expect severe fentanyl withdrawal symptoms.
How you administer fentanyl also matters. Have you been taking fentanyl patches, or do you inject fentanyl with other opioids? The latter will likely result in more severe withdrawal symptoms.
If you often combine other substances of abuse with fentanyl, this can make the withdrawal process more complicated. Data shows that approximately one-third of individuals who receive treatment for opioid use disorder also misuse alcohol.
Alcohol use combined with opioid use is a risk factor for fatal overdose and increases the risk of relapse during treatment. It is not recommended that you begin this process unsupervised, especially if you are a polydrug user, have pre-existing health conditions, or are concerned about your mental health.
Polydrug use is also commonly associated with underlying mental health disorders. For this reason, you must seek support from a professional treatment facility — one that understands the value of holistic treatment. The goal is to complete the withdrawal process and continue receiving ongoing therapy to help you address your triggers and develop healthier coping mechanisms.
Although fentanyl symptoms can be uncomfortable, not seeking help could mean the difference between life and death. This synthetic opioid has claimed far too many lives — even though support is available.
What Causes Fentanyl Withdrawal?
The way that fentanyl influences your brain is similar to other opioid drugs. Taking fentanyl targets opioid receptors in the body, many of which are found in several brain structures, including those that involve pain, the control of emotions, and reward processing.
Fentanyl’s mechanism of action is complex, involving multiple brain areas and brain chemicals, including dopamine. Since dopamine levels rise in the reward areas of your brain, this is what creates feelings of relaxation and an increased risk of addiction.
Fentanyl withdrawal typically begins with increased tolerance, leading to physical dependence. As you increase the dosage and take that dose regularly, you experience fentanyl withdrawal symptoms once you stop using.
When you take a substance away that you’re dependent on, imbalance occurs. As your brain tries to restore balance, withdrawal symptoms kick in.
Unlike prescription opioids, users taking illicitly manufactured fentanyl do not know how much they’re taking. This inconsistency makes fentanyl so dangerous — especially when other drugs are laced with it.
According to the CDC, fentanyl overdose deaths tripled among teens over the past two years (and surged five-fold among Black teens). In many of these cases, users were unaware they were taking fentanyl.
Among those who do know they are taking fentanyl, repeated use can lead to physical dependence. At this point, the fentanyl withdrawal process creates a vicious cycle of abuse. Once a physical dependence develops, even if a user wants to stop using, it can be very challenging. Psychological dependence is also a cause for concern, requiring ongoing therapy.
How Long Does Fentanyl Withdrawal Take?
To determine the duration of fentanyl withdrawal, consider the drug’s half-life. Fentanyl has a relatively short half-life of just 3-7 hours. This timeline means that within 3-7 hours, the plasma concentration of fentanyl in your body will reduce by half.
Fentanyl is a short-acting opioid, differing from long-acting opioids, like methadone. Since it is short-acting, fentanyl withdrawal symptoms generally develop within 8-24 hours after last use. In this case, you can expect more intense symptoms than long-acting opioids, but these symptoms will be briefer.
Although the fentanyl withdrawal process is highly individualized, the duration is most often between 4-10 days. However, this period only refers to physical withdrawal symptoms and may last longer depending on your circumstances.
Opioid withdrawal is commonly associated with post-acute withdrawal syndrome (PAWS). The symptoms of this syndrome are similar to those associated with mood and anxiety disorders, including insomnia, mood swings, and increased anxiety.
Approximately 90% of recovering opioid users experience the syndrome to some degree, and it can last for months — even years. Researchers believe that PAWS results from physiologic changes in the brain following drug abuse.
Brain abnormalities associated with chronic fentanyl use are what lead to dependence. Although these changes in the brain often resolve within weeks after you stop using, the abnormalities that cause addiction are long-lasting and wide-ranging.
So, to answer how long fentanyl withdrawal lasts is a tricky question. Psychological conditioning involves many variables and can prolong the withdrawal process. It is not uncommon for individuals to experience cravings that lead to relapse months or even years after they are no longer dependent.
Again, that is why it’s so important to work with a multidisciplinary team. You must have the support you need throughout the recovery process. As your goals and needs change, your treatment plan will evolve. Having access to individualized care is critical. You are a unique being, and your treatment plan should reflect that.
How to Safely Manage Fentanyl Detox
As discussed, fentanyl withdrawal is not typically life-threatening. However, it is incredibly uncomfortable — even painful.
When seeking the support of a professional clinical team, you may enter a medically-assisted detox program. Pharmacological management ensures the safest and most comfortable fentanyl withdrawal process possible. This process will begin with an initial assessment.
The goal is to understand your current needs based on your medical history and the substances you use. There is no one-size-fits-all approach, which is why the assessment period is vital. At this time, you must share any pre-existing health conditions.
Your safety is always the highest priority in a professional detoxification facility. For example, if you abuse both fentanyl and alcohol, you must share this with your care team. If you have a history of seizures, this is something they need to know. The same applies if you have a history of heart issues, as the abrupt discontinuation of long-term opioid use can lead to serious cardiac complications. So, the assessment period and willingness to work with a professional team could save your life.
During medically-assisted detox, one common intervention is the use of buprenorphine. When studied in rats, the discontinuation of fentanyl administration leads to withdrawal symptoms. The subjects were given buprenorphine, which prevented fentanyl withdrawal signs.
Similar effects are seen in humans. Before buprenorphine administration, withdrawal symptoms can be intolerable for some. So, having this option can help address one of the main barriers to treatment — distressing withdrawal symptoms. This medication has been shown to cut overdose deaths in half, allowing people to resume productive lives.
Other common medications include morphine, methadone, and tramadol. Depending on your needs, you may also be prescribed medical support, such as clonidine, to help you sleep or to address rising blood pressure.
When you gain the assistance of a professional care team, you will be monitored throughout the fentanyl withdrawal process. If your needs change, they will offer the resources and support you need to stay safe and comfortable.
It is important to note that the fentanyl withdrawal process is the first step. Most users will continue using if they do not receive ongoing support. Opioid use disorder is a complicated condition that requires continued care. The goal is to reduce the risk of relapse and improve overall well-being. Since your tolerance will decrease following the fentanyl withdrawal process, you will face an increased risk of overdose.
Holistic treatment programs will offer a range of treatment options, beginning with evidence-based therapy. Under federal law, if you are receiving medication-assisted treatment (MAT), you must also receive counseling.
The combination of MAT and counseling has been shown to be highly effective. For example, cognitive-behavioral therapy is effective as a monotherapy and as part of combination treatment strategies. This therapy option can address substance use disorder and mental health conditions.
When to Contact a Medical Professional
The first step can seem overwhelming, especially if you have tried to quit using fentanyl in the past. Fentanyl withdrawal symptoms can be daunting. However, with the proper support and access to holistic care, you can overcome your physical and psychological dependence on fentanyl and other substances of abuse.
Although your reliance on fentanyl may have become your new norm, it does not need to dictate your future. You can live a healthy, productive, and fulfilling life free from opioids. Taking a proactive approach today could save your life.
A professional substance abuse and mental health facility will offer you comprehensive, customized treatment. The top facilities provide a wide range of evidence-based treatment options, ranging from psychotherapy to meditation therapy, ensuring individualized care.
If you’re ready to take the first step toward your new life, one that is free of fentanyl, there is no better time than today. Call a professional treatment facility like Zinnia Health today.
Related Articles
- Fentanyl Use Disorder Treatment
- Fentanyl and Alcohol Substance Abuse
- Fentanyl Overdose: What You Need to Know