Benzodiazepine Abuse and Addiction Treatment Options
Most people will take a benzodiazepine at some point in life. The majority won’t even know that they have been prescribed the drug. Surgeons often use short-acting benzos to sedate patients.
These powerful drugs serve essential roles in modern medicine. They can also create severe problems when mistreated. What are benzodiazepines, and how can you know when someone has a problem with them? Keep reading to learn more and find treatment options that lead to successful, long-term recovery.

What Are Benzodiazepines?
Benzodiazepines are a class of drugs that bond with gamma-aminobutyric acid (GABA) receptors in the brain. Interacting with neurotransmitters in the central nervous system (CNS) makes them effective hypnotics, anxiolytics, and sedatives.
Common benzodiazepines include:
- Ativan (lorazepam)
- Clorazepate
- Diazepam
- Estazolam
- Flurazepam
- Halcion (triazolam)
- Klonopin (clonazepam)
- Librium (chlordiazepoxide)
- Nitrazepam
- Oxazepam
- Restoril (temazepam)
- Valium (diazepam)
- Versed (midazolam)
- Xanax (alprazolam)
The FDA has approved some benzodiazepines for short-term and long-term treatments. For example, psychiatrists might prescribe Klonopin to treat anxiety disorders and seizure disorders. Doctors often use Versed in combination with other drugs to cause sedation, decrease awareness, and lower anxiety during surgery.
Some benzodiazepines are even used to decrease the potentially life-threatening symptoms of alcohol withdrawal.
While benzos play critical roles in healthcare and mental health treatment, they also have a high abuse potential. Patients that take high doses or use them for longer than prescribed have an increased risk of addiction.
Why Do People Use Benzos?
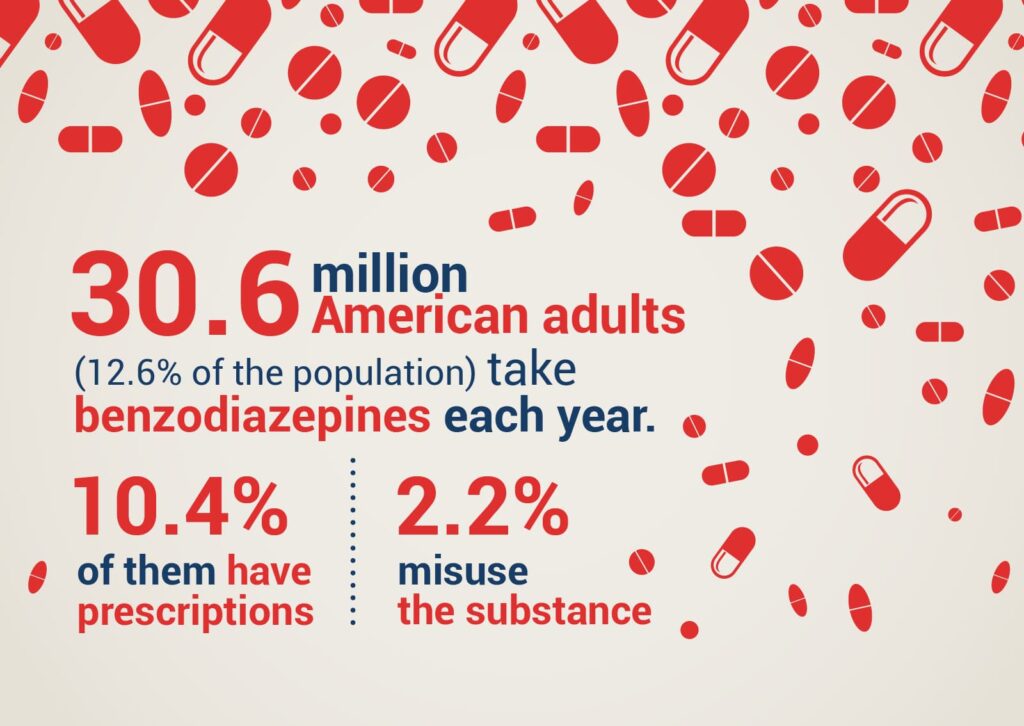
Research shows that about 30.6 million American adults (12.6% of the population) take benzodiazepines per year. Most of them (about 10.4%) have prescriptions. The other 2.2% misuse the substances.
Medical Benzo Use
Medical professionals might prescribe the drugs to help people living with conditions like:
- Generalized anxiety disorder (GAD)
- Insomnia
- Panic disorder
- Seizure disorders
- Social phobia
Drugs in this class can also keep patients calm before and during medical procedures.
Medical use of benzodiazepines is relatively safe when doctors monitor the patient’s dosage. However, the FDA recognizes that even medical use can lead to dangerous situations. In 2020, the agency announced that it would require manufacturers to include messaging about the severe risks of abuse, addiction, physical dependence, and withdrawals.
The Risk of Benzo Misuse
It is relatively easy to see why millions of people misuse benzos. A compassionate doctor might prescribe a long-acting drug like Klonopin to help someone living with panic attacks.
Unfortunately, the prescribed dosage can become less effective over time. When panic attacks return, the patient might request a higher dosage. When denied the higher dosage, some people will seek black market drugs to prevent symptoms like anxiety.
Once the patient develops a physical dependency, quitting the drugs can cause adverse effects that make success nearly impossible.
Medical detox offers a better opportunity for successfully quitting an addiction to benzos. Contact a Zinnia Health location to learn more about addressing addiction and mental health issues that might contribute to drug use.
Black Market Benzo Use
Not everyone starts taking benzos to treat medical conditions. Black market dealers might sell drugs like Xanax and Klonopin to people who want the relaxing effects of benzodiazepines.
Black market benzos could also help people tolerate the unwanted side effects of other drugs. For example, someone taking stimulants might use depressants to avoid the “crash” many people experience as the drugs wear off.
People might also combine benzos with alcohol and other drugs to get more extreme highs. This is an extremely dangerous practice. For example, mixing benzos with other depressants like alcohol and opioids could cause blackouts and respiratory failure. Overdosing on the drugs can relax the central nervous system so much that the person stops breathing.
Additional Dangers of Black Market Benzo Use
Black market benzos don’t always contain the drugs sellers advertise. Illicit manufacturers can make counterfeit pills from highly potent benzos not approved for human consumption. To make matters even more complicated, they might press pills that stamp the IDs of legitimate prescriptions onto the fraudulent drugs.
For example, a pill made from an illicit, untested chemical might have the ID “G 372 2” stamped into it. “G 372 2” is a drug ID used for 2mg pills of alprazolam made by Greenstone Limited. Stamping the ID into the pill misleads buyers into thinking they’re purchasing legitimate prescription drugs. Users don’t know what drugs they’re purchasing and ingesting. The seller might not even know.
Black market benzos can become extremely dangerous when illicit manufacturers combine drugs to make their products more potent. Someone might combine a small amount of alprazolam with fentanyl or other opioids. Putting these two depressants into one pill puts users at risk of overdose, respiratory distress, and death. Many don’t even know they have taken a deadly combination of drugs.
As governments vigilantly protect their communities from dangerous drugs, some street dealers will turn to increasingly potent options. From the dealer’s perspective, it makes sense to choose strong drugs because they can mix smaller amounts into their products. The potent chemicals are easier to distribute stealthily and make drugs more appealing to some customers. They can also put a lot at risk of overdose and addiction.
Health Effects of Benzo Abuse
Short-term use of prescribed benzodiazepines is not likely to cause any adverse health effects. It’s unlikely that you will put your health at risk by taking a small amount of Klonopin after a particularly stressful life event. Just make sure you follow your doctor’s instructions to stay safe.
Similarly, the type of benzodiazepines used during medical procedures probably will not have long-term effects on your health. The drug will have a short half-life, so it leaves your system quickly. More likely than not, you will not even remember the doctor giving you the drug.
However, long-term and recreational benzo use can lead to serious health consequences. For example, taking a large dose of Ativan could cause:
- Respiratory arrest (not breathing)
- Loss of judgment and coordination that leads to physical injury
- Increased risk of self-harm or suicide
Long-term use and addiction could contribute to health issues like:
- Liver injury or liver disease
- Sleep disruptions
- Impaired cognition
- Depression
- Anxiety
- Mania
- Psychosis
- Delirium
- Dementia
- Sexual dysfunction
- Increased cancer risk
Additionally, withdrawing from benzos presents challenges similar to withdrawing from alcohol. Withdrawal symptoms can include:
- High anxiety
- Panic attacks
- Mood swings
- Depression
- Insomnia
- Aches and pains
- Nausea and vomiting
- Hallucinations
- Grand mal seizures
Withdrawing from benzodiazepines without medical support could even lead to loss of life.
Unfortunately, the symptoms of withdrawal can last from days to months, depending on the type of benzodiazepine, dosage taken, and length of addiction.
Common Signs of Benzo Abuse
How can you tell when a loved one has a substance abuse problem? Some common signs of benzo abuse include:
- Slurred speech
- Blurred vision
- Blackouts
- Poor memory
- Excessive drowsiness or sleepiness
- Dramatic weight loss or weight gain
- Mood changes
- Avoiding social situations
- Poor judgment
- Asking other people for their benzodiazepines
- Legal consequences of doctor shopping, stealing drugs, and related activities
- Unexplained weakness
- Taking more risks than usual
- Combining benzos with alcohol and other substances
Treatment for Benzodiazepine Drug Addiction
Successful treatments for benzodiazepine addiction usually require careful planning and medical attention. The specific approach will depend on factors like:
- The type of benzodiazepines the patient uses
- Whether the patient has other substance abuse issues, such as alcohol dependence
- How long the patient has been taking drugs
- The typical dosage the patient takes
- Whether the patient has underlying mental health issues that also need treatment
Tapering Benzodiazepine Use
Many doctors agree that slow tapering is the most successful approach to treating benzodiazepine addiction. Tapering helps manage some of the most severe effects of withdrawal, such as intense anxiety. The strategy can also help avoid dangerous withdrawal effects, including grand mal seizures.
When tapering benzo use, a program might:
- Switch the patient to a drug with a long half-life, letting them take fewer pills without experiencing withdrawal symptoms. Diazepam and clonazepam often work well.
- Initially lowering the daily dose by 25-30%.
- Continuing to reduce the dose by 5-10% daily or weekly, depending on the patient’s response.
- Adding anticonvulsant drugs for patients used to taking high doses of benzodiazepines.
- Preventing insomnia by scheduling a dose before bedtime.
- Provide sleep hygiene interventions.
The amount of time it takes to taper can differ significantly from person to person. Those struggling with low-dosage addictions might only need medical attention for a couple weeks.
Those taking very large doses might need more than a month of attention. For example, the Department of Veterans Affairs uses a 15-week tapering schedule for patients taking 4 mg of lorazepam or 40 mg of diazepam daily.
People with benzo addictions might begin the detox process through in-patient services. Eventually, they can transfer to outpatient services that help them reach their goals.
Addressing Underlying Mental Health Issues
Underlying mental health issues like PTSD and panic disorder often lead people to take benzodiazepines. The drugs offer momentary relief from the symptoms of some mental health disorders. Eventually, drug-seeking behavior can lead to addiction.
Addressing underlying mental health issues could contribute to a patient’s long-term sobriety.
Prescribing antidepressants might lessen some adverse symptoms of mental health challenges. Many of them take a week or longer to have noticeable effects, though.
Cognitive-behavioral therapy (CBT) offers a more reliable, long-term solution to overcoming benzo addiction. Unfortunately, taking benzodiazepines likely hinders the effectiveness of psychotherapy. CBT offers a more pragmatic approach that can get positive results within a few sessions.
The VA says that tapering helped 25% of its patients withdraw from benzodiazepines successfully. The success rate grew to 76% when the intervention combined tapering with 10 sessions of group CBT.
Cognitive-behavioral therapy likely helps patients reach and maintain sobriety because it:
- Encourages patients to identify and confront cognitive distortions in their thinking.
- Asks patients to verbalize their thoughts so they can more accurately determine their validity.
- Teaches patients to label unhelpful thoughts into categories like “overgeneralization,” “fortune telling,” “mind reading,” “selective abstraction,” “catastrophizing,” and “emotional reasoning.”
- Uncovers the thought distortions related to each category.
- Confronts dysfunctional core beliefs, such as “I am unlovable” and “I cannot recover.”
Exposure therapy can also play a critical role in recovery, especially when patients have PTSD and phobias. Exposure therapy encourages patients to sit with uncomfortable feelings until they pass. People recovering from substance use disorder and mental health issues often use CBT techniques to endure the anxiety of exposure. For example, someone with social anxiety might confront cognitive distortions while sitting in a crowded area. Adding a rational perspective could help the person remain present even while feeling distressed. Over time, the patient experiences less distress when exposed to the anxiety-producing event or environment.
A combination of tapering, antidepressants, CBT, and exposure therapy could give someone several tools they can use to recover from addiction. An individual doesn’t need to choose one path to success. It often helps to use as many approaches as possible.
Find the Help You Need at Zinnia Health
Zinnia Health is committed to helping people struggling with benzodiazepine addiction and mental health issues recover. We have a growing network of treatment centers to meet the needs of people across North America.
If you or someone you know needs help addressing benzo abuse or addiction, contact our office via email or phone at (855) 430-9439. Thousands of people have recovered from benzo misuse. Finding the right treatment option will position you for long-term success without relying on drugs.
Related Articles
- How Long Do Benzodiazepines Stay in Your System?
- Benzos Withdrawal
- What Are the Side Effects of Benzodiazepine Abuse?

